|
Analysis Overview: COVID-19 Genetic Vaccine Safety in Children
“Even as experts expressed concern about a marked jump in hospitalizations — an increase more than double that among adults — doctors and researchers said they were not seeing evidence that Omicron was more threatening to children.
In fact, preliminary data suggests that compared with the Delta variant, Omicron appears to be causing milder illness in children, similar to early findings for adults.”
NY Times, “Omicron Is Not More Severe for Children, Despite Rising Hospitalizations” By Andrew Jacobs Dec. 28, 2021
The risk of death associated with COVID-19 in healthy children is virtually non-existent, as children have significant immunologic advantages relative to the older adult population (> 65 years) which comprises the high risk cohort for COVID-19 (see Omicron has Cracked Open the Overton Window , “We’re never going to learn about how safe this vaccine is unless we start giving it” , and COVID-19 Today).
The risk of death and disease in children has become even more rare with Omicron. Yet even prior to the advent of Omicron, a peer reviewed study clearly demonstrated (using safety data accumulated during past variant circulation) that the genetic COVID-19 vaccines carry a risk/benefit ratio of five deaths in the older, high risk cohort for every one life saved from COVID-19 (and those data did not account for the reporting bias inherent in US deaths due to COVID consequent to inappropriate use of PCR tests). See “Why are we vaccinating children against COVID-19?” (Toxicology Reports, Volume 8, 2021, Pages 1665-1684 ).
“Thus, our extremely conservative estimate for risk-benefit ratio is about 5/1. In plain English, people in the 65+ demographic are five times as likely to die from the inoculation as from COVID-19 under the most favorable assumptions! This demographic is the most vulnerable to adverse effects from COVID-19. As the age demographics go below about 35 years old, the chances of death from COVID-19 become very small, and when they go below 18, become negligible.”
The new variant of COVID-19, Omicron, has exploded onto the scene. What was already an inverted risk benefit ratio for genetic vaccination in children and adults (greater risk of death from vaccine than from COVID-19) will become even more inverted since the risks of COVID-19 are further reduced with Omicron. The Omicron variant is different in five essential ways:
- More infectious and will soon be the dominant variant in the USA
- Less pathogenic
- Poorly matched to currently available vaccines
- Natural immunity is providing good protection against Omicron
- Disease symptoms are more similar to the common cold
The issue of COVID-19 gene therapy technology -based vaccine mandates for children is a pressing issue confronting parents, grandparents, and public health officials throughout the world. Unfortunately, the topic has become highly politicized, and active censorship by legacy media outlets has made it difficult for parents and stakeholders to obtain access to the actual data required for the full informed consent prior to acceptance of a medical procedure required by law (see for example members of the Trusted News Initiative including Thompson-Reuters).
Presented on the linked website is a large collection of information and data from both primary sources and analyses which will allow parents, grandparents, and other stakeholders to make their own determination concerning the risks and benefits of the genetic COVID-19 vaccines for their children. This compilation of references, primary information, and analyses represents the collective work product of hundreds of physicians and medical scientists. It supports the consensus Physicians Declaration of the 16,000+ strong International Association of Physicians and Medical Scientists, which includes the following resolution:
…READ THE REST OF THIS ARTICLE & COMMENTS.
Canadian Covid Care Alliance shows how…
Pfizer’s own 6 month report data on its COVID-19 inoculation shows that greater illness and death in the inoculation arm than the placebo arm. Plus, poor trial design, missing data, underpowered studies, passive surveillance and more. For the PDF of this presentation visit:
…Read the full Presentation (PDF)
Covid Care Alliance’s channel on Rumble
This presentation is available in PDF and video
format on our website at
www.canadiancovidcarealliance.org
COVID-19 VACCINATION ADVERSE EVENTS THAT COULD HARM CHILDREN REFERENCES:
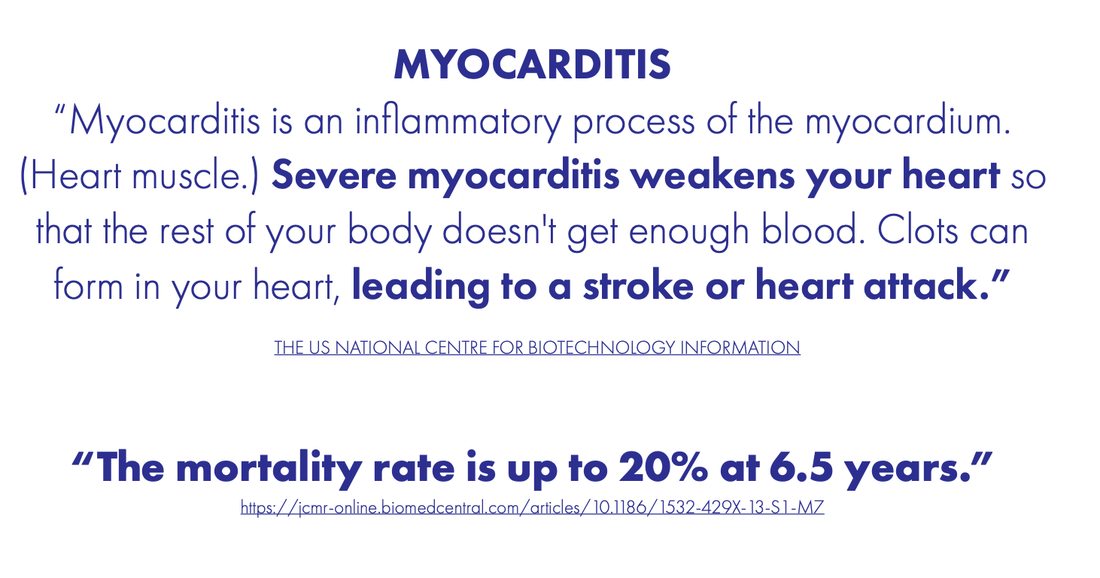
Abbate, A., Gavin, J., Madanchi, N., Kim, C., Shah, P. R., Klein, K., . . . Danielides, S. (2021). Fulminant myocarditis and systemic hyperinflammation temporally associated with BNT162b2 mRNA COVID-19 vaccination in two patients. Int J Cardiol, 340, 119-121. doi:10.1016/j.ijcard.2021.08.018. https://www.ncbi.nlm.nih.gov/pubmed/34416319
Abu Mouch, S., Roguin, A., Hellou, E., Ishai, A., Shoshan, U., Mahamid, L., . . . Berar Yanay, N. (2021). Myocarditis following COVID-19 mRNA vaccination. Vaccine, 39(29), 3790-3793. doi:10.1016/j.vaccine.2021.05.087. https://www.ncbi.nlm.nih.gov/pubmed/34092429
Albert, E., Aurigemma, G., Saucedo, J., & Gerson, D. S. (2021). Myocarditis following COVID-19 vaccination. Radiol Case Rep, 16(8), 2142-2145. doi:10.1016/j.radcr.2021.05.033. https://www.ncbi.nlm.nih.gov/pubmed/34025885
Aye, Y. N., Mai, A. S., Zhang, A., Lim, O. Z. H., Lin, N., Ng, C. H., . . . Chew, N. W. S. (2021). Acute Myocardial Infarction and Myocarditis following COVID-19 Vaccination. QJM. doi:10.1093/qjmed/hcab252. https://www.ncbi.nlm.nih.gov/pubmed/34586408
Azir, M., Inman, B., Webb, J., & Tannenbaum, L. (2021). STEMI Mimic: Focal Myocarditis in an Adolescent Patient After mRNA COVID-19 Vaccine. J Emerg Med, 61(6), e129-e132. doi:10.1016/j.jemermed.2021.09.017. https://www.ncbi.nlm.nih.gov/pubmed/34756746
Bozkurt, B., Kamat, I., & Hotez, P. J. (2021). Myocarditis With COVID-19 mRNA Vaccines. Circulation, 144(6), 471-484. doi:10.1161/CIRCULATIONAHA.121.056135. https://www.ncbi.nlm.nih.gov/pubmed/34281357
Buchhorn, R., Meyer, C., Schulze-Forster, K., Junker, J., & Heidecke, H. (2021). Autoantibody Release in Children after Corona Virus mRNA Vaccination: A Risk Factor of Multisystem Inflammatory Syndrome? Vaccines (Basel), 9(11). doi:10.3390/vaccines9111353. https://www.ncbi.nlm.nih.gov/pubmed/34835284
Calcaterra, G., Bassareo, P. P., Barilla, F., Romeo, F., & Mehta, J. L. (2022). Concerning the unexpected prothrombotic state following some coronavirus disease 2019 vaccines. J Cardiovasc Med (Hagerstown), 23(2), 71-74. doi:10.2459/JCM.0000000000001232. https://www.ncbi.nlm.nih.gov/pubmed/34366403
Calcaterra, G., Mehta, J. L., de Gregorio, C., Butera, G., Neroni, P., Fanos, V., & Bassareo, P. P. (2021). COVID 19 Vaccine for Adolescents. Concern about Myocarditis and Pericarditis. Pediatr Rep, 13(3), 530-533. doi:10.3390/pediatric13030061. https://www.ncbi.nlm.nih.gov/pubmed/34564344
Chai, Q., Nygaard, U., Schmidt, R. C., Zaremba, T., Moller, A. M., & Thorvig, C. M. (2022). Multisystem inflammatory syndrome in a male adolescent after his second Pfizer-BioNTech COVID-19 vaccine. Acta Paediatr, 111(1), 125-127. doi:10.1111/apa.16141. https://www.ncbi.nlm.nih.gov/pubmed/34617315
Chamling, B., Vehof, V., Drakos, S., Weil, M., Stalling, P., Vahlhaus, C., . . . Yilmaz, A. (2021). Occurrence of acute infarct-like myocarditis following COVID-19 vaccination: just an accidental co-incidence or rather vaccination-associated autoimmune myocarditis? Clin Res Cardiol, 110(11), 1850-1854. doi:10.1007/s00392-021-01916-w. https://www.ncbi.nlm.nih.gov/pubmed/34333695
Chan AC, Tan BY, Goh Y, Tan SS, Tambyah PA. Aseptic meningitis after BNT-162b2 COVID-19 vaccination. Brain Behav Immun Health. 2022 Feb;19:100406. doi: 10.1016/j.bbih.2021.100406. Epub 2021 Dec 13. PMID: 34927105; PMCID: PMC8667462. https://www.sciencedirect.com/science/article/pii/S266635462100209X?via%3Dihub
Chang, J. C., & Hawley, H. B. (2021). Vaccine-Associated Thrombocytopenia and Thrombosis: Venous Endotheliopathy Leading to Venous Combined Micro-Macrothrombosis. Medicina (Kaunas), 57(11). doi:10.3390/medicina57111163. https://www.ncbi.nlm.nih.gov/pubmed/34833382
Chelala, L., Jeudy, J., Hossain, R., Rosenthal, G., Pietris, N., & White, C. (2021). Cardiac MRI Findings of Myocarditis After COVID-19 mRNA Vaccination in Adolescents. AJR Am J Roentgenol. doi:10.2214/AJR.21.26853. https://www.ncbi.nlm.nih.gov/pubmed/34704459
Choi, S., Lee, S., Seo, J. W., Kim, M. J., Jeon, Y. H., Park, J. H., . . . Yeo, N. S. (2021). Myocarditis-induced Sudden Death after BNT162b2 mRNA COVID-19 Vaccination in Korea: Case Report Focusing on Histopathological Findings. J Korean Med Sci, 36(40), e286. doi:10.3346/jkms.2021.36.e286. https://www.ncbi.nlm.nih.gov/pubmed/34664804
Chouchana, L., Blet, A., Al-Khalaf, M., Kafil, T. S., Nair, G., Robblee, J., . . . Liu, P. P. (2021). Features of Inflammatory Heart Reactions Following mRNA COVID-19 Vaccination at a Global Level. Clin Pharmacol Ther. doi:10.1002/cpt.2499. https://www.ncbi.nlm.nih.gov/pubmed/34860360
Chua, G. T., Kwan, M. Y. W., Chui, C. S. L., Smith, R. D., Cheung, E. C., Tian, T., . . . Ip, P. (2021). Epidemiology of Acute Myocarditis/Pericarditis in Hong Kong Adolescents Following Comirnaty Vaccination. Clin Infect Dis. doi:10.1093/cid/ciab989. https://www.ncbi.nlm.nih.gov/pubmed/34849657
Clarke, R., & Ioannou, A. (2021). Should T2 mapping be used in cases of recurrent myocarditis to differentiate between the acute inflammation and chronic scar? J Pediatr. doi:10.1016/j.jpeds.2021.12.026. https://www.ncbi.nlm.nih.gov/pubmed/34933012
Colaneri, M., De Filippo, M., Licari, A., Marseglia, A., Maiocchi, L., Ricciardi, A., . . . Bruno, R. (2021). COVID vaccination and asthma exacerbation: might there be a link? Int J Infect Dis, 112, 243-246. doi:10.1016/j.ijid.2021.09.026. https://www.ncbi.nlm.nih.gov/pubmed/34547487
Das, B. B., Kohli, U., Ramachandran, P., Nguyen, H. H., Greil, G., Hussain, T., . . . Khan, D. (2021). Myopericarditis after messenger RNA Coronavirus Disease 2019 Vaccination in Adolescents 12 to 18 Years of Age. J Pediatr, 238, 26-32 e21. doi:10.1016/j.jpeds.2021.07.044. https://www.ncbi.nlm.nih.gov/pubmed/34339728
Deb, A., Abdelmalek, J., Iwuji, K., & Nugent, K. (2021). Acute Myocardial Injury Following COVID-19 Vaccination: A Case Report and Review of Current Evidence from Vaccine Adverse Events Reporting System Database. J Prim Care Community Health, 12, 21501327211029230. doi:10.1177/21501327211029230. https://www.ncbi.nlm.nih.gov/pubmed/34219532
Dickey, J. B., Albert, E., Badr, M., Laraja, K. M., Sena, L. M., Gerson, D. S., . . . Aurigemma, G. P. (2021). A Series of Patients With Myocarditis Following SARS-CoV-2 Vaccination With mRNA-1279 and BNT162b2. JACC Cardiovasc Imaging, 14(9), 1862-1863. doi:10.1016/j.jcmg.2021.06.003. https://www.ncbi.nlm.nih.gov/pubmed/34246585
Dimopoulou, D., Spyridis, N., Vartzelis, G., Tsolia, M. N., & Maritsi, D. N. (2021). Safety and tolerability of the COVID-19 mRNA-vaccine in adolescents with juvenile idiopathic arthritis on treatment with TNF-inhibitors. Arthritis Rheumatol. doi:10.1002/art.41977. https://www.ncbi.nlm.nih.gov/pubmed/34492161
Dimopoulou, D., Vartzelis, G., Dasoula, F., Tsolia, M., & Maritsi, D. (2021). Immunogenicity of the COVID-19 mRNA vaccine in adolescents with juvenile idiopathic arthritis on treatment with TNF inhibitors. Ann Rheum Dis. doi:10.1136/annrheumdis-2021-221607. https://www.ncbi.nlm.nih.gov/pubmed/34844930
Ehrlich, P., Klingel, K., Ohlmann-Knafo, S., Huttinger, S., Sood, N., Pickuth, D., & Kindermann, M. (2021). Biopsy-proven lymphocytic myocarditis following first mRNA COVID-19 vaccination in a 40-year-old male: case report. Clin Res Cardiol, 110(11), 1855-1859. doi:10.1007/s00392-021-01936-6. https://www.ncbi.nlm.nih.gov/pubmed/34487236
Facetti, S., Giraldi, M., Vecchi, A. L., Rogiani, S., & Nassiacos, D. (2021). [Acute myocarditis in a young adult two days after Pfizer vaccination]. G Ital Cardiol (Rome), 22(11), 891-893. doi:10.1714/3689.36746. https://www.ncbi.nlm.nih.gov/pubmed/34709227
Fazlollahi, A., Zahmatyar, M., Noori, M., Nejadghaderi, S. A., Sullman, M. J. M., Shekarriz-Foumani, R., . . . Safiri, S. (2021). Cardiac complications following mRNA COVID-19 vaccines: A systematic review of case reports and case series. Rev Med Virol, e2318. doi:10.1002/rmv.2318. https://www.ncbi.nlm.nih.gov/pubmed/34921468
Foltran, D., Delmas, C., Flumian, C., De Paoli, P., Salvo, F., Gautier, S., . . . Montastruc, F. (2021). Myocarditis and Pericarditis in Adolescents after First and Second doses of mRNA COVID-19 Vaccines. Eur Heart J Qual Care Clin Outcomes. doi:10.1093/ehjqcco/qcab090. https://www.ncbi.nlm.nih.gov/pubmed/34849667
Forgacs, D., Jang, H., Abreu, R. B., Hanley, H. B., Gattiker, J. L., Jefferson, A. M., & Ross, T. M. (2021). SARS-CoV-2 mRNA Vaccines Elicit Different Responses in Immunologically Naive and Pre-Immune Humans. Front Immunol, 12, 728021. doi:10.3389/fimmu.2021.728021. https://www.ncbi.nlm.nih.gov/pubmed/34646267
Furer, V., Eviatar, T., Zisman, D., Peleg, H., Paran, D., Levartovsky, D., . . . Elkayam, O. (2021). Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study. Ann Rheum Dis, 80(10), 1330-1338. doi:10.1136/annrheumdis-2021-220647. https://www.ncbi.nlm.nih.gov/pubmed/34127481
Gatti, M., Raschi, E., Moretti, U., Ardizzoni, A., Poluzzi, E., & Diemberger, I. (2021). Influenza Vaccination and Myo-Pericarditis in Patients Receiving Immune Checkpoint Inhibitors: Investigating the Likelihood of Interaction through the Vaccine Adverse Event Reporting System and VigiBase. Vaccines (Basel), 9(1). doi:10.3390/vaccines9010019. https://www.ncbi.nlm.nih.gov/pubmed/33406694
Gautam, N., Saluja, P., Fudim, M., Jambhekar, K., Pandey, T., & Al’Aref, S. (2021). A Late Presentation of COVID-19 Vaccine-Induced Myocarditis. Cureus, 13(9), e17890. doi:10.7759/cureus.17890. https://www.ncbi.nlm.nih.gov/pubmed/34660088
Gellad, W. F. (2021). Myocarditis after vaccination against covid-19. BMJ, 375, n3090. doi:10.1136/bmj.n3090. https://www.ncbi.nlm.nih.gov/pubmed/34916217
Greenhawt, M., Abrams, E. M., Shaker, M., Chu, D. K., Khan, D., Akin, C., . . . Golden, D. B. K. (2021). The Risk of Allergic Reaction to SARS-CoV-2 Vaccines and Recommended Evaluation and Management: A Systematic Review, Meta-Analysis, GRADE Assessment, and International Consensus Approach. J Allergy Clin Immunol Pract, 9(10), 3546-3567. doi:10.1016/j.jaip.2021.06.006. https://www.ncbi.nlm.nih.gov/pubmed/34153517
Hasnie, A. A., Hasnie, U. A., Patel, N., Aziz, M. U., Xie, M., Lloyd, S. G., & Prabhu, S. D. (2021). Perimyocarditis following first dose of the mRNA-1273 SARS-CoV-2 (Moderna) vaccine in a healthy young male: a case report. BMC Cardiovasc Disord, 21(1), 375. doi:10.1186/s12872-021-02183-3. https://www.ncbi.nlm.nih.gov/pubmed/34348657
Hause, A. M., Gee, J., Baggs, J., Abara, W. E., Marquez, P., Thompson, D., . . . Shay, D. K. (2021). COVID-19 Vaccine Safety in Adolescents Aged 12-17 Years – United States, December 14, 2020-July 16, 2021. MMWR Morb Mortal Wkly Rep, 70(31), 1053-1058. doi:10.15585/mmwr.mm7031e1. https://www.ncbi.nlm.nih.gov/pubmed/34351881
Helms, J. M., Ansteatt, K. T., Roberts, J. C., Kamatam, S., Foong, K. S., Labayog, J. S., & Tarantino, M. D. (2021). Severe, Refractory Immune Thrombocytopenia Occurring After SARS-CoV-2 Vaccine. J Blood Med, 12, 221-224. doi:10.2147/JBM.S307047. https://www.ncbi.nlm.nih.gov/pubmed/33854395
Hippisley-Cox, J., Patone, M., Mei, X. W., Saatci, D., Dixon, S., Khunti, K., . . . Coupland, C. A. C. (2021). Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and SARS-CoV-2 positive testing: self-controlled case series study. BMJ, 374, n1931. doi:10.1136/bmj.n1931. https://www.ncbi.nlm.nih.gov/pubmed/34446426
Ho, J. S., Sia, C. H., Ngiam, J. N., Loh, P. H., Chew, N. W., Kong, W. K., & Poh, K. K. (2021). A review of COVID-19 vaccination and the reported cardiac manifestations. Singapore Med J. doi:10.11622/smedj.2021210. https://www.ncbi.nlm.nih.gov/pubmed/34808708
Iguchi, T., Umeda, H., Kojima, M., Kanno, Y., Tanaka, Y., Kinoshita, N., & Sato, D. (2021). Cumulative Adverse Event Reporting of Anaphylaxis After mRNA COVID-19 Vaccine (Pfizer-BioNTech) Injections in Japan: The First-Month Report. Drug Saf, 44(11), 1209-1214. doi:10.1007/s40264-021-01104-9. https://www.ncbi.nlm.nih.gov/pubmed/34347278
In brief: Myocarditis with the Pfizer/BioNTech and Moderna COVID-19 vaccines. (2021). Med Lett Drugs Ther, 63(1629), e9. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/34544112https://www.ncbi.nlm.nih.gov/pubmed/34544112
Ioannou, A. (2021a). Myocarditis should be considered in those with a troponin rise and unobstructed coronary arteries following Pfizer-BioNTech COVID-19 vaccination. QJM. doi:10.1093/qjmed/hcab231. https://www.ncbi.nlm.nih.gov/pubmed/34463755
Ioannou, A. (2021b). T2 mapping should be utilised in cases of suspected myocarditis to confirm an acute inflammatory process. QJM. doi:10.1093/qjmed/hcab326. https://www.ncbi.nlm.nih.gov/pubmed/34931681
Isaak, A., Feisst, A., & Luetkens, J. A. (2021). Myocarditis Following COVID-19 Vaccination. Radiology, 301(1), E378-E379. doi:10.1148/radiol.2021211766. https://www.ncbi.nlm.nih.gov/pubmed/34342500
Istampoulouoglou, I., Dimitriou, G., Spani, S., Christ, A., Zimmermanns, B., Koechlin, S., . . . Leuppi-Taegtmeyer, A. B. (2021). Myocarditis and pericarditis in association with COVID-19 mRNA-vaccination: cases from a regional pharmacovigilance centre. Glob Cardiol Sci Pract, 2021(3), e202118. doi:10.21542/gcsp.2021.18. https://www.ncbi.nlm.nih.gov/pubmed/34805376
Jain, S. S., Steele, J. M., Fonseca, B., Huang, S., Shah, S., Maskatia, S. A., . . . Grosse-Wortmann, L. (2021). COVID-19 Vaccination-Associated Myocarditis in Adolescents. Pediatrics, 148(5). doi:10.1542/peds.2021-053427. https://www.ncbi.nlm.nih.gov/pubmed/34389692
Jhaveri, R., Adler-Shohet, F. C., Blyth, C. C., Chiotos, K., Gerber, J. S., Green, M., . . . Zaoutis, T. (2021). Weighing the Risks of Perimyocarditis With the Benefits of SARS-CoV-2 mRNA Vaccination in Adolescents. J Pediatric Infect Dis Soc, 10(10), 937-939. doi:10.1093/jpids/piab061. https://www.ncbi.nlm.nih.gov/pubmed/34270752
Kaneta, K., Yokoi, K., Jojima, K., Kotooka, N., & Node, K. (2021). Young Male With Myocarditis Following mRNA-1273 Vaccination Against Coronavirus Disease-2019 (COVID-19). Circ J. doi:10.1253/circj.CJ-21-0818. https://www.ncbi.nlm.nih.gov/pubmed/34744118
Kaul, R., Sreenivasan, J., Goel, A., Malik, A., Bandyopadhyay, D., Jin, C., . . . Panza, J. A. (2021). Myocarditis following COVID-19 vaccination. Int J Cardiol Heart Vasc, 36, 100872. doi:10.1016/j.ijcha.2021.100872. https://www.ncbi.nlm.nih.gov/pubmed/34568540
Khogali, F., & Abdelrahman, R. (2021). Unusual Presentation of Acute Perimyocarditis Following SARS-COV-2 mRNA-1237 Moderna Vaccination. Cureus, 13(7), e16590. doi:10.7759/cureus.16590. https://www.ncbi.nlm.nih.gov/pubmed/34447639
Kim, H. W., Jenista, E. R., Wendell, D. C., Azevedo, C. F., Campbell, M. J., Darty, S. N., . . . Kim, R. J. (2021). Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination. JAMA Cardiol, 6(10), 1196-1201. doi:10.1001/jamacardio.2021.2828. https://www.ncbi.nlm.nih.gov/pubmed/34185046
Kim, I. C., Kim, H., Lee, H. J., Kim, J. Y., & Kim, J. Y. (2021). Cardiac Imaging of Acute Myocarditis Following COVID-19 mRNA Vaccination. J Korean Med Sci, 36(32), e229. doi:10.3346/jkms.2021.36.e229. https://www.ncbi.nlm.nih.gov/pubmed/34402228
King, W. W., Petersen, M. R., Matar, R. M., Budweg, J. B., Cuervo Pardo, L., & Petersen, J. W. (2021). Myocarditis following mRNA vaccination against SARS-CoV-2, a case series. Am Heart J Plus, 8, 100042. doi:10.1016/j.ahjo.2021.100042. https://www.ncbi.nlm.nih.gov/pubmed/34396358
Klein, N. P., Lewis, N., Goddard, K., Fireman, B., Zerbo, O., Hanson, K. E., . . . Weintraub, E. S. (2021). Surveillance for Adverse Events After COVID-19 mRNA Vaccination. JAMA, 326(14), 1390-1399. doi:10.1001/jama.2021.15072. https://www.ncbi.nlm.nih.gov/pubmed/34477808
Klimek, L., Bergmann, K. C., Brehler, R., Pfutzner, W., Zuberbier, T., Hartmann, K., . . . Worm, M. (2021). Practical handling of allergic reactions to COVID-19 vaccines: A position paper from German and Austrian Allergy Societies AeDA, DGAKI, GPA and OGAI. Allergo J Int, 1-17. doi:10.1007/s40629-021-00165-7. https://www.ncbi.nlm.nih.gov/pubmed/33898162
Klimek, L., Novak, N., Hamelmann, E., Werfel, T., Wagenmann, M., Taube, C., . . . Worm, M. (2021). Severe allergic reactions after COVID-19 vaccination with the Pfizer/BioNTech vaccine in Great Britain and USA: Position statement of the German Allergy Societies: Medical Association of German Allergologists (AeDA), German Society for Allergology and Clinical Immunology (DGAKI) and Society for Pediatric Allergology and Environmental Medicine (GPA). Allergo J Int, 30(2), 51-55. doi:10.1007/s40629-020-00160-4. https://www.ncbi.nlm.nih.gov/pubmed/33643776
Kohli, U., Desai, L., Chowdhury, D., Harahsheh, A. S., Yonts, A. B., Ansong, A., . . . Ang, J. Y. (2021). mRNA Coronavirus-19 Vaccine-Associated Myopericarditis in Adolescents: A Survey Study. J Pediatr. doi:10.1016/j.jpeds.2021.12.025. https://www.ncbi.nlm.nih.gov/pubmed/34952008
Kostoff, R. N., Calina, D., Kanduc, D., Briggs, M. B., Vlachoyiannopoulos, P., Svistunov, A. A., & Tsatsakis, A. (2021a). Erratum to “Why are we vaccinating children against COVID-19?” [Toxicol. Rep. 8C (2021) 1665-1684 / 1193]. Toxicol Rep, 8, 1981. doi:10.1016/j.toxrep.2021.10.003. https://www.ncbi.nlm.nih.gov/pubmed/34642628
Kostoff, R. N., Calina, D., Kanduc, D., Briggs, M. B., Vlachoyiannopoulos, P., Svistunov, A. A., & Tsatsakis, A. (2021b). Why are we vaccinating children against COVID-19? Toxicol Rep, 8, 1665-1684. doi:10.1016/j.toxrep.2021.08.010. https://www.ncbi.nlm.nih.gov/pubmed/34540594
Kwan, M. Y. W., Chua, G. T., Chow, C. B., Tsao, S. S. L., To, K. K. W., Yuen, K. Y., . . . Ip, P. (2021). mRNA COVID vaccine and myocarditis in adolescents. Hong Kong Med J, 27(5), 326-327. doi:10.12809/hkmj215120. https://www.ncbi.nlm.nih.gov/pubmed/34393110
Lee, E., Chew, N. W. S., Ng, P., & Yeo, T. J. (2021). Reply to “Letter to the editor: Myocarditis should be considered in those with a troponin rise and unobstructed coronary arteries following PfizerBioNTech COVID-19 vaccination”. QJM. doi:10.1093/qjmed/hcab232. https://www.ncbi.nlm.nih.gov/pubmed/34463770
Lee, E. J., Cines, D. B., Gernsheimer, T., Kessler, C., Michel, M., Tarantino, M. D., . . . Bussel, J. B. (2021). Thrombocytopenia following Pfizer and Moderna SARS-CoV-2 vaccination. Am J Hematol, 96(5), 534-537. doi:10.1002/ajh.26132. https://www.ncbi.nlm.nih.gov/pubmed/33606296
Levin, D., Shimon, G., Fadlon-Derai, M., Gershovitz, L., Shovali, A., Sebbag, A., . . . Gordon, B. (2021). Myocarditis following COVID-19 vaccination – A case series. Vaccine, 39(42), 6195-6200. doi:10.1016/j.vaccine.2021.09.004. https://www.ncbi.nlm.nih.gov/pubmed/34535317
Li, M., Yuan, J., Lv, G., Brown, J., Jiang, X., & Lu, Z. K. (2021). Myocarditis and Pericarditis following COVID-19 Vaccination: Inequalities in Age and Vaccine Types. J Pers Med, 11(11). doi:10.3390/jpm11111106. https://www.ncbi.nlm.nih.gov/pubmed/34834458
Lim, Y., Kim, M. C., Kim, K. H., Jeong, I. S., Cho, Y. S., Choi, Y. D., & Lee, J. E. (2021). Case Report: Acute Fulminant Myocarditis and Cardiogenic Shock After Messenger RNA Coronavirus Disease 2019 Vaccination Requiring Extracorporeal Cardiopulmonary Resuscitation. Front Cardiovasc Med, 8, 758996. doi:10.3389/fcvm.2021.758996. https://www.ncbi.nlm.nih.gov/pubmed/34778411
Long, S. S. (2021). Important Insights into Myopericarditis after the Pfizer mRNA COVID-19 Vaccination in Adolescents. J Pediatr, 238, 5. doi:10.1016/j.jpeds.2021.07.057. https://www.ncbi.nlm.nih.gov/pubmed/34332972
Luk, A., Clarke, B., Dahdah, N., Ducharme, A., Krahn, A., McCrindle, B., . . . McDonald, M. (2021). Myocarditis and Pericarditis After COVID-19 mRNA Vaccination: Practical Considerations for Care Providers. Can J Cardiol, 37(10), 1629-1634. doi:10.1016/j.cjca.2021.08.001. https://www.ncbi.nlm.nih.gov/pubmed/34375696
Madelon, N., Lauper, K., Breville, G., Sabater Royo, I., Goldstein, R., Andrey, D. O., . . . Eberhardt, C. S. (2021). Robust T cell responses in anti-CD20 treated patients following COVID-19 vaccination: a prospective cohort study. Clin Infect Dis. doi:10.1093/cid/ciab954. https://www.ncbi.nlm.nih.gov/pubmed/34791081
Mangat, C., & Milosavljevic, N. (2021). BNT162b2 Vaccination during Pregnancy Protects Both the Mother and Infant: Anti-SARS-CoV-2 S Antibodies Persistently Positive in an Infant at 6 Months of Age. Case Rep Pediatr, 2021, 6901131. doi:10.1155/2021/6901131. https://www.ncbi.nlm.nih.gov/pubmed/34676123
Mark, C., Gupta, S., Punnett, A., Upton, J., Orkin, J., Atkinson, A., . . . Alexander, S. (2021). Safety of administration of BNT162b2 mRNA (Pfizer-BioNTech) COVID-19 vaccine in youths and young adults with a history of acute lymphoblastic leukemia and allergy to PEG-asparaginase. Pediatr Blood Cancer, 68(11), e29295. doi:10.1002/pbc.29295. https://www.ncbi.nlm.nih.gov/pubmed/34398511
McLean, K., & Johnson, T. J. (2021). Myopericarditis in a previously healthy adolescent male following COVID-19 vaccination: A case report. Acad Emerg Med, 28(8), 918-921. doi:10.1111/acem.14322. https://www.ncbi.nlm.nih.gov/pubmed/34133825
Mevorach, D., Anis, E., Cedar, N., Bromberg, M., Haas, E. J., Nadir, E., . . . Alroy-Preis, S. (2021). Myocarditis after BNT162b2 mRNA Vaccine against Covid-19 in Israel. N Engl J Med, 385(23), 2140-2149. doi:10.1056/NEJMoa2109730. https://www.ncbi.nlm.nih.gov/pubmed/34614328
Minocha, P. K., Better, D., Singh, R. K., & Hoque, T. (2021). Recurrence of Acute Myocarditis Temporally Associated with Receipt of the mRNA Coronavirus Disease 2019 (COVID-19) Vaccine in a Male Adolescent. J Pediatr, 238, 321-323. doi:10.1016/j.jpeds.2021.06.035. https://www.ncbi.nlm.nih.gov/pubmed/34166671
Mohamed, L., Madsen, A. M. R., Schaltz-Buchholzer, F., Ostenfeld, A., Netea, M. G., Benn, C. S., & Kofoed, P. E. (2021). Reactivation of BCG vaccination scars after vaccination with mRNA-Covid-vaccines: two case reports. BMC Infect Dis, 21(1), 1264. doi:10.1186/s12879-021-06949-0. https://www.ncbi.nlm.nih.gov/pubmed/34930152
Montgomery, J., Ryan, M., Engler, R., Hoffman, D., McClenathan, B., Collins, L., . . . Cooper, L. T., Jr. (2021). Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military. JAMA Cardiol, 6(10), 1202-1206. doi:10.1001/jamacardio.2021.2833. https://www.ncbi.nlm.nih.gov/pubmed/34185045
Murakami, Y., Shinohara, M., Oka, Y., Wada, R., Noike, R., Ohara, H., . . . Ikeda, T. (2021). Myocarditis Following a COVID-19 Messenger RNA Vaccination: A Japanese Case Series. Intern Med. doi:10.2169/internalmedicine.8731-21. https://www.ncbi.nlm.nih.gov/pubmed/34840235
Nagasaka, T., Koitabashi, N., Ishibashi, Y., Aihara, K., Takama, N., Ohyama, Y., . . . Kaneko, Y. (2021). Acute Myocarditis Associated with COVID-19 Vaccination: A Case Report. J Cardiol Cases. doi:10.1016/j.jccase.2021.11.006. https://www.ncbi.nlm.nih.gov/pubmed/34876937
Ntouros, P. A., Vlachogiannis, N. I., Pappa, M., Nezos, A., Mavragani, C. P., Tektonidou, M. G., . . . Sfikakis, P. P. (2021). Effective DNA damage response after acute but not chronic immune challenge: SARS-CoV-2 vaccine versus Systemic Lupus Erythematosus. Clin Immunol, 229, 108765. doi:10.1016/j.clim.2021.108765. https://www.ncbi.nlm.nih.gov/pubmed/34089859
Nygaard, U., Holm, M., Bohnstedt, C., Chai, Q., Schmidt, L. S., Hartling, U. B., . . . Stensballe, L. G. (2022). Population-based Incidence of Myopericarditis After COVID-19 Vaccination in Danish Adolescents. Pediatr Infect Dis J, 41(1), e25-e28. doi:10.1097/INF.0000000000003389. https://www.ncbi.nlm.nih.gov/pubmed/34889875
Park, H., Yun, K. W., Kim, K. R., Song, S. H., Ahn, B., Kim, D. R., . . . Kim, Y. J. (2021). Epidemiology and Clinical Features of Myocarditis/Pericarditis before the Introduction of mRNA COVID-19 Vaccine in Korean Children: a Multicenter Study. J Korean Med Sci, 36(32), e232. doi:10.3346/jkms.2021.36.e232. https://www.ncbi.nlm.nih.gov/pubmed/34402230
Park, J., Brekke, D. R., & Bratincsak, A. (2021). Self-limited myocarditis presenting with chest pain and ST segment elevation in adolescents after vaccination with the BNT162b2 mRNA vaccine. Cardiol Young, 1-4. doi:10.1017/S1047951121002547. https://www.ncbi.nlm.nih.gov/pubmed/34180390
Patel, Y. R., Louis, D. W., Atalay, M., Agarwal, S., & Shah, N. R. (2021). Cardiovascular magnetic resonance findings in young adult patients with acute myocarditis following mRNA COVID-19 vaccination: a case series. J Cardiovasc Magn Reson, 23(1), 101. doi:10.1186/s12968-021-00795-4. https://www.ncbi.nlm.nih.gov/pubmed/34496880
Patone, M., Mei, X. W., Handunnetthi, L., Dixon, S., Zaccardi, F., Shankar-Hari, M., . . . Hippisley-Cox, J. (2021). Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. doi:10.1038/s41591-021-01630-0. https://www.ncbi.nlm.nih.gov/pubmed/34907393
Patrignani, A., Schicchi, N., Calcagnoli, F., Falchetti, E., Ciampani, N., Argalia, G., & Mariani, A. (2021). Acute myocarditis following Comirnaty vaccination in a healthy man with previous SARS-CoV-2 infection. Radiol Case Rep, 16(11), 3321-3325. doi:10.1016/j.radcr.2021.07.082. https://www.ncbi.nlm.nih.gov/pubmed/34367386
Perez, Y., Levy, E. R., Joshi, A. Y., Virk, A., Rodriguez-Porcel, M., Johnson, M., . . . Swift, M. D. (2021). Myocarditis Following COVID-19 mRNA Vaccine: A Case Series and Incidence Rate Determination. Clin Infect Dis. doi:10.1093/cid/ciab926. https://www.ncbi.nlm.nih.gov/pubmed/34734240
Perrotta, A., Biondi-Zoccai, G., Saade, W., Miraldi, F., Morelli, A., Marullo, A. G., . . . Peruzzi, M. (2021). A snapshot global survey on side effects of COVID-19 vaccines among healthcare professionals and armed forces with a focus on headache. Panminerva Med, 63(3), 324-331. doi:10.23736/S0031-0808.21.04435-9. https://www.ncbi.nlm.nih.gov/pubmed/34738774
Sanchez Tijmes, F., Thavendiranathan, P., Udell, J. A., Seidman, M. A., & Hanneman, K. (2021). Cardiac MRI Assessment of Nonischemic Myocardial Inflammation: State of the Art Review and Update on Myocarditis Associated with COVID-19 Vaccination. Radiol Cardiothorac Imaging, 3(6), e210252. doi:10.1148/ryct.210252. https://www.ncbi.nlm.nih.gov/pubmed/34934954
Schauer, J., Buddhe, S., Colyer, J., Sagiv, E., Law, Y., Mallenahalli Chikkabyrappa, S., & Portman, M. A. (2021). Myopericarditis After the Pfizer Messenger Ribonucleic Acid Coronavirus Disease Vaccine in Adolescents. J Pediatr, 238, 317-320. doi:10.1016/j.jpeds.2021.06.083. https://www.ncbi.nlm.nih.gov/pubmed/34228985
Schneider, J., Sottmann, L., Greinacher, A., Hagen, M., Kasper, H. U., Kuhnen, C., . . . Schmeling, A. (2021). Postmortem investigation of fatalities following vaccination with COVID-19 vaccines. Int J Legal Med, 135(6), 2335-2345. doi:10.1007/s00414-021-02706-9. https://www.ncbi.nlm.nih.gov/pubmed/34591186
Schramm, R., Costard-Jackle, A., Rivinius, R., Fischer, B., Muller, B., Boeken, U., . . . Gummert, J. (2021). Poor humoral and T-cell response to two-dose SARS-CoV-2 messenger RNA vaccine BNT162b2 in cardiothoracic transplant recipients. Clin Res Cardiol, 110(8), 1142-1149. doi:10.1007/s00392-021-01880-5. https://www.ncbi.nlm.nih.gov/pubmed/34241676
Sessa, F., Salerno, M., Esposito, M., Di Nunno, N., Zamboni, P., & Pomara, C. (2021). Autopsy Findings and Causality Relationship between Death and COVID-19 Vaccination: A Systematic Review. J Clin Med, 10(24). doi:10.3390/jcm10245876. https://www.ncbi.nlm.nih.gov/pubmed/34945172
Sharif, N., Alzahrani, K. J., Ahmed, S. N., & Dey, S. K. (2021). Efficacy, Immunogenicity and Safety of COVID-19 Vaccines: A Systematic Review and Meta-Analysis. Front Immunol, 12, 714170. doi:10.3389/fimmu.2021.714170. https://www.ncbi.nlm.nih.gov/pubmed/34707602
Shazley, O., & Alshazley, M. (2021). A COVID-Positive 52-Year-Old Man Presented With Venous Thromboembolism and Disseminated Intravascular Coagulation Following Johnson & Johnson Vaccination: A Case-Study. Cureus, 13(7), e16383. doi:10.7759/cureus.16383. https://www.ncbi.nlm.nih.gov/pubmed/34408937
Shiyovich, A., Witberg, G., Aviv, Y., Eisen, A., Orvin, K., Wiessman, M., . . . Hamdan, A. (2021). Myocarditis following COVID-19 vaccination: magnetic resonance imaging study. Eur Heart J Cardiovasc Imaging. doi:10.1093/ehjci/jeab230. https://www.ncbi.nlm.nih.gov/pubmed/34739045
Simone, A., Herald, J., Chen, A., Gulati, N., Shen, A. Y., Lewin, B., & Lee, M. S. (2021). Acute Myocarditis Following COVID-19 mRNA Vaccination in Adults Aged 18 Years or Older. JAMA Intern Med, 181(12), 1668-1670. doi:10.1001/jamainternmed.2021.5511. https://www.ncbi.nlm.nih.gov/pubmed/34605853
Singer, M. E., Taub, I. B., & Kaelber, D. C. (2021). Risk of Myocarditis from COVID-19 Infection in People Under Age 20: A Population-Based Analysis. medRxiv. doi:10.1101/2021.07.23.21260998. https://www.ncbi.nlm.nih.gov/pubmed/34341797
Smith, C., Odd, D., Harwood, R., Ward, J., Linney, M., Clark, M., . . . Fraser, L. K. (2021). Deaths in children and young people in England after SARS-CoV-2 infection during the first pandemic year. Nat Med. doi:10.1038/s41591-021-01578-1. https://www.ncbi.nlm.nih.gov/pubmed/34764489
Snapiri, O., Rosenberg Danziger, C., Shirman, N., Weissbach, A., Lowenthal, A., Ayalon, I., . . . Bilavsky, E. (2021). Transient Cardiac Injury in Adolescents Receiving the BNT162b2 mRNA COVID-19 Vaccine. Pediatr Infect Dis J, 40(10), e360-e363. doi:10.1097/INF.0000000000003235. https://www.ncbi.nlm.nih.gov/pubmed/34077949
Spinner, J. A., Julien, C. L., Olayinka, L., Dreyer, W. J., Bocchini, C. E., Munoz, F. M., & Devaraj, S. (2021). SARS-CoV-2 anti-spike antibodies after vaccination in pediatric heart transplantation: A first report. J Heart Lung Transplant. doi:10.1016/j.healun.2021.11.001. https://www.ncbi.nlm.nih.gov/pubmed/34911654
Starekova, J., Bluemke, D. A., Bradham, W. S., Grist, T. M., Schiebler, M. L., & Reeder, S. B. (2021). Myocarditis Associated with mRNA COVID-19 Vaccination. Radiology, 301(2), E409-E411. doi:10.1148/radiol.2021211430. https://www.ncbi.nlm.nih.gov/pubmed/34282971
Sulemankhil, I., Abdelrahman, M., & Negi, S. I. (2021). Temporal association between the COVID-19 Ad26.COV2.S vaccine and acute myocarditis: A case report and literature review. Cardiovasc Revasc Med. doi:10.1016/j.carrev.2021.08.012. https://www.ncbi.nlm.nih.gov/pubmed/34420869
Tailor, P. D., Feighery, A. M., El-Sabawi, B., & Prasad, A. (2021). Case report: acute myocarditis following the second dose of mRNA-1273 SARS-CoV-2 vaccine. Eur Heart J Case Rep, 5(8), ytab319. doi:10.1093/ehjcr/ytab319. https://www.ncbi.nlm.nih.gov/pubmed/34514306https://www.ncbi.nlm.nih.gov/pubmed/34955479
Team, C. C.-R., Food, & Drug, A. (2021). Allergic Reactions Including Anaphylaxis After Receipt of the First Dose of Pfizer-BioNTech COVID-19 Vaccine – United States, December 14-23, 2020. MMWR Morb Mortal Wkly Rep, 70(2), 46-51. doi:10.15585/mmwr.mm7002e1. https://www.ncbi.nlm.nih.gov/pubmed/33444297
Tinoco, M., Leite, S., Faria, B., Cardoso, S., Von Hafe, P., Dias, G., . . . Lourenco, A. (2021). Perimyocarditis Following COVID-19 Vaccination. Clin Med Insights Cardiol, 15, 11795468211056634. doi:10.1177/11795468211056634. https://www.ncbi.nlm.nih.gov/pubmed/34866957
Truong, D. T., Dionne, A., Muniz, J. C., McHugh, K. E., Portman, M. A., Lambert, L. M., . . . Newburger, J. W. (2021). Clinically Suspected Myocarditis Temporally Related to COVID-19 Vaccination in Adolescents and Young Adults. Circulation. doi:10.1161/CIRCULATIONAHA.121.056583. https://www.ncbi.nlm.nih.gov/pubmed/34865500
Umei, T. C., Kishino, Y., Shiraishi, Y., Inohara, T., Yuasa, S., & Fukuda, K. (2021). Recurrence of myopericarditis following mRNA COVID-19 vaccination in a male adolescent. CJC Open. doi:10.1016/j.cjco.2021.12.002. https://www.ncbi.nlm.nih.gov/pubmed/34904134
Vidula, M. K., Ambrose, M., Glassberg, H., Chokshi, N., Chen, T., Ferrari, V. A., & Han, Y. (2021). Myocarditis and Other Cardiovascular Complications of the mRNA-Based COVID-19 Vaccines. Cureus, 13(6), e15576. doi:10.7759/cureus.15576. https://www.ncbi.nlm.nih.gov/pubmed/34277198
Visclosky, T., Theyyunni, N., Klekowski, N., & Bradin, S. (2021). Myocarditis Following mRNA COVID-19 Vaccine. Pediatr Emerg Care, 37(11), 583-584. doi:10.1097/PEC.0000000000002557. https://www.ncbi.nlm.nih.gov/pubmed/34731877
Warren, C. M., Snow, T. T., Lee, A. S., Shah, M. M., Heider, A., Blomkalns, A., . . . Nadeau, K. C. (2021). Assessment of Allergic and Anaphylactic Reactions to mRNA COVID-19 Vaccines With Confirmatory Testing in a US Regional Health System. JAMA Netw Open, 4(9), e2125524. doi:10.1001/jamanetworkopen.2021.25524.
Watkins, K., Griffin, G., Septaric, K., & Simon, E. L. (2021). Myocarditis after BNT162b2 vaccination in a healthy male. Am J Emerg Med, 50, 815 e811-815 e812. doi:10.1016/j.ajem.2021.06.051. https://www.ncbi.nlm.nih.gov/pubmed/34229940https://www.ncbi.nlm.nih.gov/pubmed/34336774
Welsh, K. J., Baumblatt, J., Chege, W., Goud, R., & Nair, N. (2021). Thrombocytopenia including immune thrombocytopenia after receipt of mRNA COVID-19 vaccines reported to the Vaccine Adverse Event Reporting System (VAERS). Vaccine, 39(25), 3329-3332. doi:10.1016/j.vaccine.2021.04.054. https://www.ncbi.nlm.nih.gov/pubmed/34006408
Witberg, G., Barda, N., Hoss, S., Richter, I., Wiessman, M., Aviv, Y., . . . Kornowski, R. (2021). Myocarditis after Covid-19 Vaccination in a Large Health Care Organization. N Engl J Med, 385(23), 2132-2139. doi:10.1056/NEJMoa2110737. https://www.ncbi.nlm.nih.gov/pubmed/34614329
Zimmermann, P., & Curtis, N. (2020). Why is COVID-19 less severe in children? A review of the proposed mechanisms underlying the age-related difference in severity of SARS-CoV-2 infections. Arch Dis Child. doi:10.1136/archdischild-2020-320338. https://www.ncbi.nlm.nih.gov/pubmed/33262177
Guillain-Barre Syndrome (GBS) and COVID-19 Vaccination References (As GBS affects all age cohorts – references are all age cohorts)
Allen, C. M., Ramsamy, S., Tarr, A. W., Tighe, P. J., Irving, W. L., Tanasescu, R., & Evans, J. R. (2021). Guillain-Barre Syndrome Variant Occurring after SARS-CoV-2 Vaccination. Ann Neurol, 90(2), 315-318. doi:10.1002/ana.26144. https://www.ncbi.nlm.nih.gov/pubmed/34114269
Bouattour, N., Hdiji, O., Sakka, S., Fakhfakh, E., Moalla, K., Daoud, S., . . . Mhiri, C. (2021). Guillain-Barre syndrome following the first dose of Pfizer-BioNTech COVID-19 vaccine: case report and review of reported cases. Neurol Sci. doi:10.1007/s10072-021-05733-x. https://www.ncbi.nlm.nih.gov/pubmed/34796417
Censcak, D., Ungermann, L., Stetkarova, I., & Ehler, E. (2021). Guillan-Barre Syndrome after First Vaccination Dose against COVID-19: Case Report. Acta Medica (Hradec Kralove), 64(3), 183-186. doi:10.14712/18059694.2021.31. https://www.ncbi.nlm.nih.gov/pubmed/34779385
da Silva, G. F., da Silva, C. F., Oliveira, R., Romancini, F., Mendes, R. M., Locks, A., . . . Braatz, V. L. (2021). Guillain-Barre syndrome after coronavirus disease 2019 vaccine: A temporal association. Clin Exp Neuroimmunol. doi:10.1111/cen3.12678. https://www.ncbi.nlm.nih.gov/pubmed/34900000
Guillain-Barre Syndrome Eight Days after Vector-Based COVID-19 Vaccination. Case Rep Infect Dis, 2021, 3619131. doi:10.1155/2021/3619131. https://www.ncbi.nlm.nih.gov/pubmed/34055430
Finsterer, J. (2021b). Guillain-Barre syndrome 15 days after COVID-19 despite SARS-CoV-2 vaccination. IDCases, 25, e01226. doi:10.1016/j.idcr.2021.e01226. https://www.ncbi.nlm.nih.gov/pubmed/34290962
Finsterer, J. (2021d). SARS-CoV-2 vaccinations may not only be complicated by GBS but also by distal small fibre neuropathy. J Neuroimmunol, 360, 577703. doi:10.1016/j.jneuroim.2021.577703. https://www.ncbi.nlm.nih.gov/pubmed/34525410
Finsterer, J. (2022). Neurological side effects of SARS-CoV-2 vaccinations. Acta Neurol Scand, 145(1), 5-9. doi:10.1111/ane.13550. https://www.ncbi.nlm.nih.gov/pubmed/34750810
Finsterer, J., Scorza, F. A., & Scorza, C. A. (2021). Post SARS-CoV-2 vaccination Guillain-Barre syndrome in 19 patients. Clinics (Sao Paulo), 76, e3286. doi:10.6061/clinics/2021/e3286. https://www.ncbi.nlm.nih.gov/pubmed/34644738
Hasan, T., Khan, M., Khan, F., & Hamza, G. (2021). Case of Guillain-Barre syndrome following COVID-19 vaccine. BMJ Case Rep, 14(6). doi:10.1136/bcr-2021-243629. https://www.ncbi.nlm.nih.gov/pubmed/34187803
Kanabar, G., & Wilkinson, P. (2021). Guillain-Barre syndrome presenting with facial diplegia following COVID-19 vaccination in two patients. BMJ Case Rep, 14(10). doi:10.1136/bcr-2021-244527. https://www.ncbi.nlm.nih.gov/pubmed/34649856
Koike, H., Chiba, A., & Katsuno, M. (2021). Emerging Infection, Vaccination, and Guillain-Barre Syndrome: A Review. Neurol Ther, 10(2), 523-537. doi:10.1007/s40120-021-00261-4. https://www.ncbi.nlm.nih.gov/pubmed/34117994
Koike, H., & Katsuno, M. (2021). Emerging infectious diseases, vaccines and Guillain-Barre syndrome. Clin Exp Neuroimmunol. doi:10.1111/cen3.12644. https://www.ncbi.nlm.nih.gov/pubmed/34230841
Kripalani, Y., Lakkappan, V., Parulekar, L., Shaikh, A., Singh, R., & Vyas, P. (2021). A Rare Case of Guillain-Barre Syndrome following COVID-19 Vaccination. Eur J Case Rep Intern Med, 8(9), 002707. doi:10.12890/2021_002797. https://www.ncbi.nlm.nih.gov/pubmed/34671572
Leung, C. (2021). Guillain-Barre syndrome should be monitored upon mass vaccination against SARS-CoV-2. Hum Vaccin Immunother, 17(9), 2957-2958. doi:10.1080/21645515.2021.1922061. https://www.ncbi.nlm.nih.gov/pubmed/34032555
Maramattom, B. V., Krishnan, P., Paul, R., Padmanabhan, S., Cherukudal Vishnu Nampoothiri, S., Syed, A. A., & Mangat, H. S. (2021). Guillain-Barre Syndrome following ChAdOx1-S/nCoV-19 Vaccine. Ann Neurol, 90(2), 312-314. doi:10.1002/ana.26143. https://www.ncbi.nlm.nih.gov/pubmed/34114256
McKean, N., & Chircop, C. (2021). Guillain-Barre syndrome after COVID-19 vaccination. BMJ Case Rep, 14(7). doi:10.1136/bcr-2021-244125. https://www.ncbi.nlm.nih.gov/pubmed/34330729
Min, Y. G., Ju, W., Ha, Y. E., Ban, J. J., Lee, S. A., Sung, J. J., & Shin, J. Y. (2021). Sensory Guillain-Barre syndrome following the ChAdOx1 nCov-19 vaccine: Report of two cases and review of literature. J Neuroimmunol, 359, 577691. doi:10.1016/j.jneuroim.2021.577691. https://www.ncbi.nlm.nih.gov/pubmed/34416410
Mokhashi, N., Narla, G., & Marchionni, C. (2021). Guillain-Barre Syndrome in a Patient With Asymptomatic Coronavirus Disease 2019 Infection and Major Depressive Disorder. Cureus, 13(3), e14161. doi:10.7759/cureus.14161. https://www.ncbi.nlm.nih.gov/pubmed/33927956
Morehouse, Z. P., Paulus, A., Jasti, S. A., & Bing, X. (2021). A Rare Variant of Guillain-Barre Syndrome Following Ad26.COV2.S Vaccination. Cureus, 13(9), e18153. doi:10.7759/cureus.18153. https://www.ncbi.nlm.nih.gov/pubmed/34703690
Nasuelli, N. A., De Marchi, F., Cecchin, M., De Paoli, I., Onorato, S., Pettinaroli, R., . . . Godi, L. (2021). A case of acute demyelinating polyradiculoneuropathy with bilateral facial palsy after ChAdOx1 nCoV-19 vaccine. Neurol Sci, 42(11), 4747-4749. doi:10.1007/s10072-021-05467-w. https://www.ncbi.nlm.nih.gov/pubmed/34272622
Nishiguchi, Y., Matsuyama, H., Maeda, K., Shindo, A., & Tomimoto, H. (2021). Miller Fisher syndrome following BNT162b2 mRNA coronavirus 2019 vaccination. BMC Neurol, 21(1), 452. doi:10.1186/s12883-021-02489-x. https://www.ncbi.nlm.nih.gov/pubmed/3478919
Oo, W. M., Giri, P., & de Souza, A. (2021). AstraZeneca COVID-19 vaccine and Guillain- Barre Syndrome in Tasmania: A causal link? J Neuroimmunol, 360, 577719. doi:10.1016/j.jneuroim.2021.577719. https://www.ncbi.nlm.nih.gov/pubmed/34560365
Prasad, A., Hurlburt, G., Podury, S., Tandon, M., Kingree, S., & Sriwastava, S. (2021). A Novel Case of Bifacial Diplegia Variant of Guillain-Barre Syndrome Following Janssen COVID-19 Vaccination. Neurol Int, 13(3), 404-409. doi:10.3390/neurolint13030040. https://www.ncbi.nlm.nih.gov/pubmed/34449715
Razok, A., Shams, A., Almeer, A., & Zahid, M. (2021). Post-COVID-19 vaccine Guillain-Barre syndrome; first reported case from Qatar. Ann Med Surg (Lond), 67, 102540. doi:10.1016/j.amsu.2021.102540. https://www.ncbi.nlm.nih.gov/pubmed/34249353
Rosenblum, H. G., Hadler, S. C., Moulia, D., Shimabukuro, T. T., Su, J. R., Tepper, N. K., . . . Oliver, S. E. (2021). Use of COVID-19 Vaccines After Reports of Adverse Events Among Adult Recipients of Janssen (Johnson & Johnson) and mRNA COVID-19 Vaccines (Pfizer-BioNTech and Moderna): Update from the Advisory Committee on Immunization Practices – United States, July 2021. MMWR Morb Mortal Wkly Rep, 70(32), 1094-1099. doi:10.15585/mmwr.mm7032e4. https://www.ncbi.nlm.nih.gov/pubmed/34383735
Rossetti, A., Gheihman, G., O’Hare, M., & Kosowsky, J. M. (2021). Guillain-Barre Syndrome Presenting as Facial Diplegia after COVID-19 Vaccination: A Case Report. J Emerg Med, 61(6), e141-e145. doi:10.1016/j.jemermed.2021.07.062. https://www.ncbi.nlm.nih.gov/pubmed/34538679
Samudralwar, R. D. (2021). Commentary: The spectrum of neurological manifestations related to COVID-19 and vaccinations. J Neuroimmunol, 358, 577660. doi:10.1016/j.jneuroim.2021.577660. https://www.ncbi.nlm.nih.gov/pubmed/34274719
Scendoni, R., Petrelli, C., Scaloni, G., & Logullo, F. O. (2021). Electromyoneurography and laboratory findings in a case of Guillain-Barre syndrome after second dose of Pfizer COVID-19 vaccine. Hum Vaccin Immunother, 1-4. doi:10.1080/21645515.2021.1954826. https://www.ncbi.nlm.nih.gov/pubmed/34347563
Sebghati, M., & Khalil, A. (2021). Uptake of vaccination in pregnancy. Best Pract Res Clin Obstet Gynaecol, 76, 53-65. doi:10.1016/j.bpobgyn.2021.03.007. https://www.ncbi.nlm.nih.gov/pubmed/33965331
Shao, S. C., Wang, C. H., Chang, K. C., Hung, M. J., Chen, H. Y., & Liao, S. C. (2021). Guillain-Barre Syndrome Associated with COVID-19 Vaccination. Emerg Infect Dis, 27(12), 3175-3178. doi:10.3201/eid2712.211634. https://www.ncbi.nlm.nih.gov/pubmed/34648420
Shasha, D., Bareket, R., Sikron, F. H., Gertel, O., Tsamir, J., Dvir, D., . . . Zacay, G. (2022). Real-world safety data for the Pfizer BNT162b2 SARS-CoV-2 vaccine: historical cohort study. Clin Microbiol Infect, 28(1), 130-134. doi:10.1016/j.cmi.2021.09.018. https://www.ncbi.nlm.nih.gov/pubmed/34592420
Sriwastava, S., Shrestha, A. K., Khalid, S. H., Colantonio, M. A., Nwafor, D., & Srivastava, S. (2021). Spectrum of Neuroimaging Findings in Post-COVID-19 Vaccination: A Case Series and Review of Literature. Neurol Int, 13(4), 622-639. doi:10.3390/neurolint13040061. https://www.ncbi.nlm.nih.gov/pubmed/34842783
Tutar, N. K., Eyigurbuz, T., Yildirim, Z., & Kale, N. (2021). A variant of Guillain-Barre syndrome after SARS-CoV-2 vaccination: AMSAN. Ideggyogy Sz, 74(7-08), 286-288. doi:10.18071/isz.74.0286. https://www.ncbi.nlm.nih.gov/pubmed/34370408
Woo, E. J., Mba-Jonas, A., Dimova, R. B., Alimchandani, M., Zinderman, C. E., & Nair, N. (2021). Association of Receipt of the Ad26.COV2.S COVID-19 Vaccine With Presumptive Guillain-Barre Syndrome, February-July 2021. JAMA, 326(16), 1606-1613. doi:10.1001/jama.2021.16496. https://www.ncbi.nlm.nih.gov/pubmed/34617967